RAKETENSTARKE PARTNER

THE FUTURE OF ORAL HEALTH
Die Zukunft in Ihrer Praxis. Der aMMP-8-Biomarker (aktive Matrix-Metalloproteinase- 8 = Kollagenase 8) ist der weltweit führende Biomarker zur Vorhersage von oralen Gewebeabbauprozessen.
Messbar machen, was nie zuvor messbar war. Mit einer Genauigkeit von 94 % bis zu fünf Jahre vor Eintreten von irreparablen Schäden (Guarnieri et.al.).
Personalized Precision Dentistry aMMP-8 & Vitamin D
Oral Fitness. Echte Prävention, die Patientenbindung schafft.
Der Traum einer präventiven Zahnmedizin für lebenslang gesunde Zähne und Zahnimplantate kann Wirklichkeit werden.


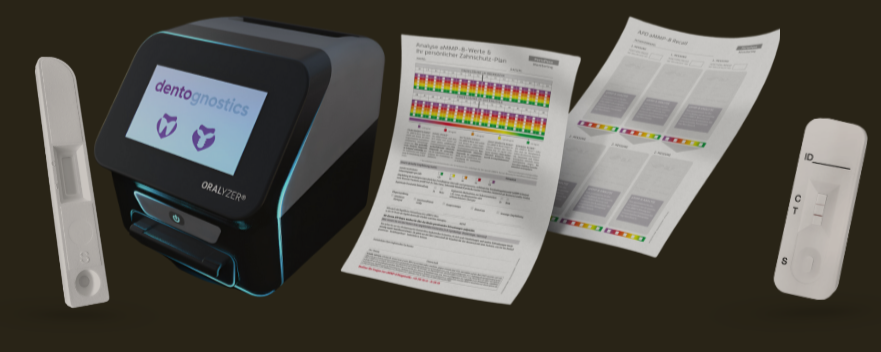
Ergebnis in 5 Minuten
Mit unserem modernen ORALyzer EXPERT® bestimmen Sie die für die orale Fitness relevanten Werte aMMP-8 und Vitamin D schnell, sicher und präzise in nur 5 Minuten direkt am Point of Care.
Persönlicher Therapieplan
Ihr Patient erhält einen individuellen Therapieplan, den Sie auf der Basis seines Oral Fitness Scores erstellen. Dieser erhält evidenzbasierte Empfehlungen was Ihr Patient tun kann, um seine Mundgesundheit selbst in die Hand zu nehmen.
Sicherung der Recall-Frequenz
Einmal eingesetzt, werden
Sie eine unübertroffene Bereitschaft Ihrer Patienten erleben, sich an die Behandlungsempfehlungen zu halten und langfristig in der Erhaltungstherapie zu bleiben.
SCREENING & MONITORING GANZHEITLICHER ORALER FITNESS

Mouth-Body-Biomarker aMMP-8
Oral-systemische Gesundheit
Implantat-Gesundheit
Vitamin D-Spiegel
WERDEN SIE TEIL DER MISSION
UNSERE TECHNOLOGIEN & PRODUKTE
DIE FASZINATION VON ECHTEM VERTRAUEN
Entdecken Sie den Effekt echter Prävention auf die Bindung und das Vertrauen Ihrer Patienten. Mit aMMP-8 kann der Traum von lebenslang gesunden Zähnen Wirklichkeit werden.
Binnen weniger Minuten erhalten Ihre Patienten einen personalisierten Therapieplan, der die Zahngesundheit und die Recall-Frequenz sichert.
WAS EXPERTEN SAGEN
Prof. Dr. Bernd Kleine-Gunk
Präsident GSAAM Germany
(Deutsche Gesellschaft für Prävention und AntiAging Medizin e.V.)
Najib N. R. Nassar
Facharzt für Reproduktionsmedizin Kinderwunschspezialist